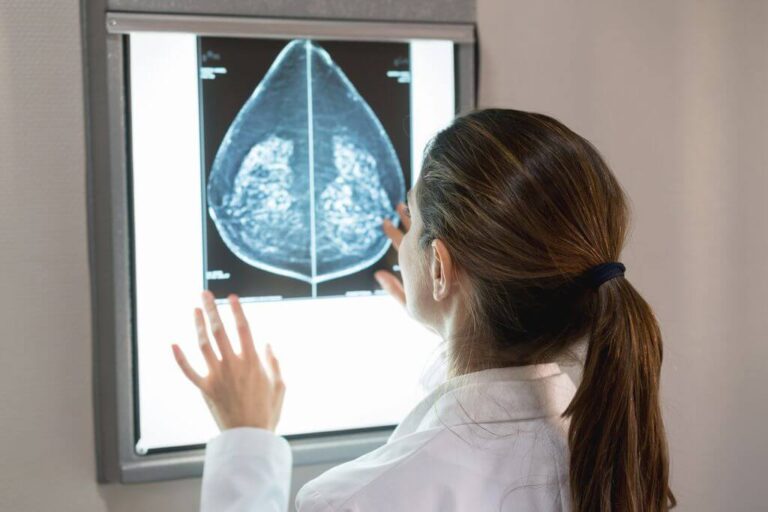
Translation of the mammography answer or its interpretation
Today, most women are familiar with mammography imaging. However, most women do not understand the results of mammography or interpretation of their mammography responses. In this article, we are going to familiarize you with a standard mammography response reporting scale so that you can know the general results of your mammography scan, however little. Keep in mind that having information about this article does not guarantee the definitive results of your mammography and you should see your doctor to interpret the results.
The purpose of writing a mammography report is to establish a relationship between a radiologist who performs your mammography with the doctor who prescribed mammography for you. However, this report is often available to you and you may want to understand it better.
A doctor named Radiologist classifies your mammography results using a numbering system. This classification system is called BI-RADS.

What is bi-rads evaluation category?
Doctors use a standard system to describe mammography findings and results. This system (called breast imaging reporting and data system or BI-RADS) sorts the results into categories 0 to 6.
With these categories, doctors can describe what they find in mammography using similar words and terms. This makes it easier to communicate about mammography scan results and follow-up after testing.
(Note: The same bi-RADS categories can also be used to describe the results of breast ultrasound or breast MRI. However, the recommended next steps after these scans may vary slightly.)
What do BI-RADS categories mean?
The table below shows the full description of the category number, definition and description of each category on the BI-RADS scale.
| Category Number | Definition | Explain |
| 0 | Incomplete – Additional imaging evaluation and/or comparison with previous mammography (or other imaging tests) is required. | This number means that the radiologist may have seen a possible malformation, but it is unclear and you will need more tests, such as other mammography using spot compression (applying compression in the smaller area when performing mammography), enlarged views, special views. Mammography views and/or ultrasound. This may indicate that the radiologist wants to compare your new mammography with older mammography to see if there have been changes in the area over time. |
| 1 | Negative | This number represents a normal scanning result. Your breasts look the same (they are symmetrical) without mass, distortion structures or suspected calcification. In this negative case, nothing new or abnormal was found. |
| 2 | Benign findings (non-cancerous) | This category also represents a negative test result (there are no signs of cancer), but the radiologist describes a finding that it is not cancer, such as benign calcifications, lumps or lymph nodes in the breast. This result can also be used to describe changes caused by a previous procedure (such as a biopsy) in the breast. This result ensures that others who look at mammography in the future do not interpret benign findings as questionable. |
| 3 | Probably benign findings – follow-up is suggested in a short timeframe | The findings in this category show that there is a very low probability (less than 2%) of cancer and these lesions are not expected to change over time. But since it hasn’t been proven to be benign, it’s very helpful to see if the area changes over time.
You will probably need to follow up with re-imaging within 6 to 12 months and regularly afterwards until the finding is proven (usually at least 2 years). This approach helps prevent unnecessary biopsies, but if the area changes over time, it still allows for early detection. |
| 4 | Suspected abnormality – biopsy should be considered | These findings certainly don’t resemble cancer, but they can be cancer. The radiologist is concerned enough to recommend a biopsy. The findings of this category can be suspicious of a wide range of tissue surfaces. For this reason, this category is often more divided:
4A: Find with a low chance of cancer (more than 2% but not more than 10%)
4B: Find out with an average chance of cancer (more than 10% but not more than 50%).
4C: Find with a high probability of cancer (more than 50% but less than 95%), but not as much as Category 5 |
| 5 | Strongly suggests malignancy – appropriate measures must be taken | The findings are similar to cancer and have a high probability of cancer (at least 95%). Biopsies are highly recommended. |
| 6 | Known malignancy proven with biopsy – appropriate measures must be taken | This category is only used for mammography (or ultrasound or MRI) findings that have previously shown them to be cancerous with a previous biopsy. Imaging may be used to observe the rate of cancer’s response to treatment. |
BI-RADS also reports breast density
Your mammography report also includes an assessment of your breast density, which describes the amount of fibrous and glandular tissue in the breasts compared to adipose tissue.
The denser your breasts, the harder it is to see abnormal areas in mammography. (Having dense breasts also slightly increases the risk of breast cancer.)
But let’s get more familiar with some of the terms and questions in this area.

What is Calcification?
Calcifications are calcium deposits in breast tissue. They are very common and the majority are non-cancerous. When many microcalcifications (small calcium profiles) are seen in one area, they are called a calcification group.
What are clip markers or clamp markers and why is it used during biopsies?
After mammography screening, there are a small percentage of women who may need additional diagnostic imaging. This is called a call. If the patient is called, additional imaging will be performed and only about 2% of women may need a biopsy. During the biopsy, a radiologist with breast imaging expertise places a small metal clamp on the breast to determine the location of the biopsy if further testing is needed.
Is tomosynthesis a better screening tool?
Yes. Compared to 2D mammography, tomosynthesis provides a clearer picture of each breast layer, which provides more visibility for the radiologist. Tomosynthesis allows for more cancers to be seen and fewer false alarms.
What should I do if I noticed abnormal changes or symptoms even after mammography became normal?
Breast self-examination is important because it allows you to know your breasts and their “normal” appearance. If you notice abnormal symptoms or changes in your breast tissue, follow up on further tests. Don’t ignore abnormal breast changes or symptoms such as secretion or mass, but keep in mind that several lifestyle changes, such as weight gain, weight loss, hormonal changes and hormonal replacement therapy, can cause your breast to change.
If my breast cancer is diagnosed, should my children do mammography at an early age?
Yes, but depending on the child’s age, ultrasound or MRI scan may be a better option. Consult your primary care doctor.
What does breast asymmetry mean in mammography report?
Breast asymmetry refers to the appearance of part of the breast tissue compared to the residuals in the other breast. The radiologist examines mammography to examine the differences in position, volume and form of breasts. In most cases, breasts are generally symmetrical in terms of density and structure, but sometimes a report may show asymmetric density, which is common and usually asymmetric.
However, radiologists may decide to undergo further tests if there are asymmetrical changes in breast tissue, as this could also represent an important finding.
What does fibroglandular density mean?
Fibroglandular tissue refers to areas in the breast that contain milk glands and milk ducts. Fibroglandular density refers to the scattered areas of density in the breast, which is a natural tissue in combination with fat.
My mammography described my breasts as “heterogeneously dense, which may hide small lumps.” What does it mean?
That means you have a relatively dense tissue that is common and not a concern. Sometimes, dense tissue can make it difficult to accurately read mammography. You and your doctor can discuss additional screening options (i.e. screening procedures in addition to mammography) if necessary.

Final word on mammography and mammography turn
Mammography is one of the best diagnostic imaging methods in the field of screening and diagnosis of breast cancer. Remember that if you want to go to the mammography center to do a mammography, be sure to have one with you. Try to take turns from the nearest mammography center.
To do this, you can easily book your appointment from the nearest mammography center through a medical scan. In the scan of medicine, you can know exactly how to do mammography,
take a mammography turn
and see your mammography response.